Osteomyelitis of the lower and upper jaw: causes, symptoms and treatment
Osteomyelitis is infectious, is classified into several main types and is most often manifested in the male part of the population. The tactics for treating jaw osteomyelitis depend on the severity of the symptoms and etiology of the disease.
Content
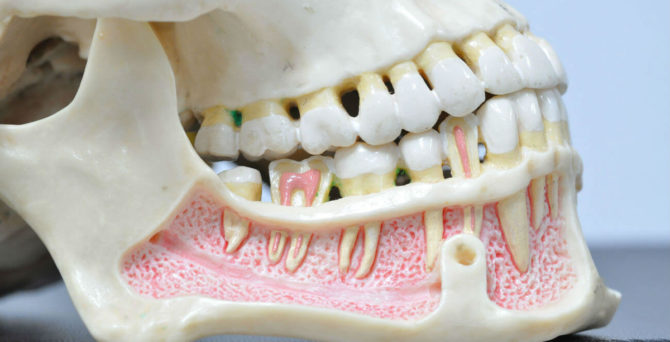
What is osteomyelitis of the jaw
Osteomyelitis in dentistry is an inflammation of the bone tissue of the jaw of an infectious and purulent nature. Pathogens include:
- staphylococci;
- E. coli;
- tubercle bacillus;
- rickettsia;
- streptococci;
- Pseudomonas aeruginosa;
- Klebsiella;
- gram-negative bacteria;
- viruses.
Most often, streptococcal and staphylococcal infections of the jaw tissue are found. Often, the disease leads to a generalization of the infection, which causes infection of the entire skeletal system of a person and tissues located nearby.
Osteomyelitis is a multifactorial disease, the probability of its development is affected by:
- infection by pathogenic microorganisms;
- the state of the immune system;
- violation of local blood circulation.
Causes of occurrence
Maxillary osteomyelitis occurs due to the penetration of pathogenic bacteria or viruses into the body. The further course of the disease depends on the state of human immunity. If it is in order, then the disease goes into a chronic stage or does not develop at all. But with immunodeficiency, the inflammatory process will begin to progress.
What diseases provoke osteomyelitis
All causes of osteomyelitis can be divided into several varieties:
| The name of the group of causes of the disease | Description |
|---|---|
| Odontogenic |
The source of infection is a bad tooth. Harmful substances enter the bone through the pulp when:
|
| Hematogenous |
Pathogens enter the skeletal system from the primary source of inflammation:
|
| Traumatic |
|
| Beam | They are associated with oncological formations in the maxillofacial region and with subsequent chemical and radiation therapy. Cells can develop into cancerous ones. |
| Toxic | Against the background of taking narcotic drugs. |
The tactics of treatment depend on an accurate diagnosis, but for any type of pathology, you must first destroy the source of inflammation, and only then act on organs and systems that were infected a second time. If the patient suffers from diabetes mellitus, pathology of the blood-forming organs or cancer, the prognosis worsens.
Osteomyelitis after tooth extraction
Osteomyelitis can occur after tooth extraction. In this case, the infection enters the hole due to insufficient quality of treatment of the oral cavity.Pathogens enter the bone tissue from the hole. One of the main signs of the disease is increased mobility of the teeth located next to the hole.
Osteomyelitis in the presence of deciduous teeth
The carious cavity in the milk tooth, which was not cured in time, can also cause the development of pathology. Moreover, the infection often destroys the rudiments of the main tooth, so if any problems with primary teeth appear, they should be treated quickly, and not hope that they will fall out soon. Milk teeth are also removed if they become a source of inflammation in the body.
Types and symptoms of jaw osteomyelitis
The symptomatology of the disease depends on the location of the focus of infection, the type and form of the pathology. With osteomyelitis of the upper jaw, radiative pains in the eyeball, temple or ear can be attributed to the symptoms of the development of pathology, and in case of mandibular pathology the pain gives to the neck or even to the shoulder.
Odontogenic
In dentistry, conventional odontogenic osteomyelitis is considered the most common form of the disease. This disease occurs as a complication of dental pathologies.
Symptoms of pathology are:
- a sharp increase in temperature;
- swelling of the face, especially at the edge of the orbit;
- enlarged lymph nodes;
- the appearance of pus in the nasal passages;
- the appearance of fistulous passages;
- sore face on palpation.
Traumatic
The main symptoms of traumatic osteomyelitis are:
- severe chills;
- the allocation of exudate from the site of injury;
- pain in the wound area;
- intoxication of the body.
The most common symptoms of osteomyelitis of the lower jaw are swelling and the appearance of a false joint. The false joint occurs due to a violation of the regenerative process of bone tissue after a fracture. Fragments are connected by loose tissue, not callus, which is why they are loosely fixed to each other.
In the early stages of the pathology, the clinical picture may be erased due to trauma, it begins to appear actively only 3-5 days after infection.
Hematogenous
The development of hematogenous osteomyelitis is associated with the ingress of pathogenic microflora into the jaw from another inflamed area.
Symptoms:
- lethargy;
- swelling of the mucosa;
- heat;
- pallor of the skin;
- the appearance of fistulas;
- general intoxication of the body.
The disease is often accompanied by inflammation of the bones of the entire skull and damage to some internal organs.
Acute form of the disease
Acute jaw osteomyelitis occurs suddenly and is characterized by general and local symptoms. Signs of the disease include:
- temperature increase up to 40 ° C;
- pallor of the skin;
- severe pain at the location of the pathogenic tooth, over time they lose a clear localization and extend to the entire jaw;
- loosening of a painful tooth;
- sudden weakness;
- arthritis of the jaw joint;
- pain when swallowing;
- fetid breath;
- swelling and hyperemia of soft tissues;
- excessive sweating;
- pronounced asymmetry of the face;
- enlarged lymph nodes.
In the presence of these symptoms, differential diagnosis is indicated:
- with a specific form of tuberculosis, syphilis or actinomycosis;
- with purulent periostitis;
- with oncological diseases of the jaw.
Chronic form
Chronic osteomyelitis is formed against the background of an acute form of the disease and strong immunity. Sometimes the disease goes into a chronic stage due to improperly selected treatment. Symptoms of pathology:
-
persistent subfebrile condition;
- severe pallor of the skin;
- lethargy;
- insomnia;
- the presence of fistulas on the face and in the oral cavity;
- swelling of the mucous membranes;
- pathological tooth mobility (one or more);
- severe pain during exacerbation.
Diagnostics
Before starting treatment, laboratory tests are required, based on them, you can determine the presence of inflammation in the body:
| Type of laboratory test | What comes to light |
|---|---|
| Blood analysis |
|
| Analysis of urine |
Availability is determined:
|
| Bone puncture (applies only to children) |
Comprises:
|
| Roentgenography |
Shows the classic signs of osteomyelitis:
|
Treatment of osteomyelitis with inflammation of the jaw bone
Treatment depends on the etiology and symptoms of the disease. It should include the following types of therapy:
- antibacterial;
- immunomodulatory;
- desensitizing.
If there is no way to cure the disease with tablets, surgery is indicated.
You can take painkillers only after consulting a doctor, uncontrolled intake of such drugs can lead to serious complications. These drugs are aimed at relieving pain, and not at eliminating the focus of infection.
Antibiotics for osteomyelitis
Antibiotics are prescribed for osteomyelitis of the jaw before surgery and sanitation of the infection site, which helps to accelerate the process of inhibition of pathogens and prevent their active reproduction.
Classification
The following antibacterial drugs are most often used to treat osteomyelitis:
- penicillins: Amoxicillin, Benzylpenicillin, Nafcillin;
- cephalosorins are especially effective against staphylococcal osteomyelitis: ceftriaxone, cefuroxime;
- fluoroquinols: Levofloxacin, Ciprofloxacin;
- aminoglycosides: Amikacin, Torbamycin;
- glycopeptides: vancomycin, teicoplanin.
To prevent the development of mycotic (fungal) infection, in addition to antibiotics, Fluconazole, Nystatin, or Ketoconazole should be taken.
Probiotics after antibiotics
After a course of antibiotics, probiotics are shown:
- monocomponent: Lactobacterin, Bifidumbacterin, Baktisporin;
- multicomponent: Bifilong, Acylact, Acinol, Linex;
- combined: Bifilis, Bifidumbacterin forte.
Surgical treatment in a dental clinic
Surgical treatment of osteomyelitis consists of various steps that are performed depending on the clinic of the disease and the results of a comprehensive examination. These include:
- Radical surgical treatment: sequestrectomy, sequestrectomy, trepanation of the long bone, resection of the jaw bone.
- Osteosynthesis
- Replacing cavities with vascularized tissues.
- Treatment of soft tissue defects.
- Surgical treatment of the site of infection.
- Removal of a tooth.
Operations for osteomyelitis are performed in all major cities of Russia (not only in Moscow or St. Petersburg). Before agreeing to surgery, it is advisable to request a license from the clinic for manipulations of such a plan.
Local therapy
Immediately after surgery, it is necessary to treat the surface of the wound with antiseptics - Levosin, Khinifuril, Iodopyron or Miramistin. In addition, foaming aerosols Dioxizole and Aminitrozole, as well as wound coverings (sterile sheets) Algimaf, Gentatsikol and Algipor should be used.Such treatment will help prevent postoperative purulent inflammation of the jaw.
Physiotherapy
The most effective methods of physiotherapy for diseases of the jaw include:
- electrophoresis with antibiotic solutions;
- ultra high frequency therapy;
- UV exposure.
Traditional medicine
Traditional medicine is an optional part of the comprehensive treatment of osteomyelitis. This disease can not be treated at home with lotions from herbs, but the following remedies can be used to relieve some inflammatory symptoms (subject to suitable antibacterial therapy and doctor’s permission):
- mummy;
- propolis and bee products;
- a solution of soda and salt;
- herbal decoctions.
These funds have a mild therapeutic effect, but they can be used in the complex treatment of osteomyelitis, since they practically have no side effects.
Complications
If you do not treat primary or chronic osteomyelitis of the upper and lower jaw, the disease can lead to serious complications:
- infection of the soft tissues of the face, neck and even back;
- sepsis and generalization of infection;
- inflammation of the orbital region, which can lead to loss of vision;
- meningitis.
If you choose the wrong method of treatment, osteomyelitis can develop into osteonecrosis - the death of bone cells, so you can not delay the appeal to the doctor.
Other diseases of the jaw in humans
Osteomyelitis of the jaw can be confused with other diseases, the most common:
| Disease name | Definition | Short description |
|---|---|---|
| Osteitis | Inflammation of bone tissue outside the periodontal tooth. | As an independent disease, osteitis does not exist for long, it quickly develops into periostitis. |
| Periostitis | Inflammation of the periosteum. | It is acute and chronic, purulent and serous. A purulent form of the disease develops as a complication of purulent periodontitis, serous - due to injuries. Purulent periostitis is accompanied by a fusion of soft tissues and periosteum, which leads to the formation of fistulas. |
| Sepsis | Infectious inflammation of bone tissue. | It occurs due to the presence of a focus of infection in the body, often leading to the death of the patient. |
| Cyst | A cavity on the root of the tooth or in the bone itself with or without epithelial lining. | They have odontogenic (due to dental diseases) and non-odogenic genesis. |
| Fibrotic dysplasia | The formation of a benign tumor. | The process is accompanied by a significant deformation of the shape of the face. The causes of the disease are unknown, doctors do not exclude the effect of heredity. |
| Osteosarcoma, chondrosarcoma, lymphoma | Malignant tumors. | They develop in any bone tissue and even in the jaw. |
At the slightest suspicion of osteomyelitis of the bone tissue of the upper or lower jaw, you need to contact the dentists, without waiting for the intensification of symptoms and the occurrence of complications. It is better to remove the problem tooth, and not wait for the formation of edema or tumor. In addition, signs of malaise may indicate a more serious disease that only a doctor can detect.