Causes, symptoms, treatment and prevention of gingivitis
Gingivitis - one of the types inflammation of the mucous membrane of the gums. A common phenomenon observed in both adults and children. Gums are the foundation of the tooth, their health determines the full functioning of the teeth themselves. Therefore, any symptoms of gingivitis should cause a mandatory visit to the dental office.
Content
What is gingivitis
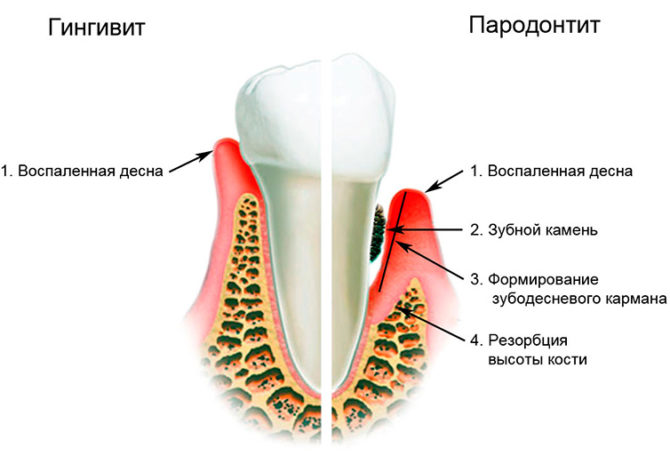
Gingivitis (from lat. gingivitis) - an inflammatory disease of the gingival tissue, which is localized in the interdental space, without affecting the dento-bone joints (mobility does not appear in the teeth). In case of untimely or poor-quality treatment, gingivitis can progress to the next stage of gum mucosa inflammation - periodontitis, in which destruction of the gingival attachments is observed. The disease is most characteristic for countries with low socio-economic status, poor-quality dental services.
Gingivitis, the symptoms and treatment of which in adults and children are practically the same, is a disease of superficial tissues. It can practically do no harm to health, but with inappropriate therapy can provoke tooth loss.
Causes of gingivitis
The mucous membrane of the gums can become inflamed for many reasons, due to internal and external factors: excessive reproduction of pathological microflora, trauma to the gum tissue, vitamin deficiency.
Microorganism development
 In the oral cavity there is always a certain number of microorganisms of various classes: bacteria, fungi, viruses. The existing balance of microflora is supported by the body’s immune system and depends on the lifestyle and human health. Some factors can cause an increase in the growth of pathogenic microflora:
In the oral cavity there is always a certain number of microorganisms of various classes: bacteria, fungi, viruses. The existing balance of microflora is supported by the body’s immune system and depends on the lifestyle and human health. Some factors can cause an increase in the growth of pathogenic microflora:
- non-compliance with the rules of oral hygiene;
- the presence of dental plaque: soft or mineralized plaque;
- untreated carious teeth;
- decreased immune defense of the body;
- the presence of inflammatory or systemic diseases of the internal organs;
- bad habits (smoking).
Gum tissue injury
Damage as a factor in the development of gingivitis is characteristic of both children and adults. The appearance of microtraumas is possible when teething, visiting a dental office, exposure to chemical or mechanical agents, radiation therapy, burns, wearing braces, poor-quality fillings or crowns.
Avitaminosis
Inadequate intake of vitamins and minerals with food or due to some diseases can lead not only to a deterioration in immunity, but also provoke pathologies in the structure of gum tissue.
Is gingivitis contagious
Gingivitis is contagious or not - different experts have their own opinions on this. The disease does not belong to the group of those transmitted by contact or in everyday life., for example, when using common spoons, glasses. However, when several people use the same toothbrush or other dental aids, microorganisms can be transmitted.And if a person has a weak immune system, there are no skills or there is no way to observe oral hygiene, inflammatory gum disease may occur.
The clinical picture of gingivitis
Gingivitis, whose symptoms appear already in the initial stage of the disease, is characterized by swelling, tenderness of the gum tissue. Redness is observed in the area of the papillae: triangular-shaped gingival areas protruding in the interdental space. As well as the gingival margin around the tooth.
 The appearance of such signs of gingivitis as bleeding, pinpoint hemorrhages, ulcerations, and the formation of the gingival pocket are possible. A frequent companion of the disease is bad breath.
The appearance of such signs of gingivitis as bleeding, pinpoint hemorrhages, ulcerations, and the formation of the gingival pocket are possible. A frequent companion of the disease is bad breath.
The localization of inflammatory processes differs depending on the clinical case and the degree of progression of inflammation: gingivitis can affect a small area of the gums, and can spread to the mucosa of both the upper and lower jaw.
Important! If the first signs of gingivitis are present: hyperemia and swelling of the gums - a dentist consultation is necessary.
Types of Gingivitis
There are acute and chronic forms of the disease. The acute course of gingivitis is characterized by the intensity of the clinical picture, painful sensations, and a rapid increase in the inflammatory process.
The chronic form, which develops with poor-quality or untimely treatment of the disease, is characterized by a more sluggish course and mild symptoms. Relapses more often occur in adults than in children in the winter and spring, when the frequency of colds increases, and a seasonal decrease in immunity is noted.
Depending on the severity and neglect of gingivitis, the disease can go through several stages:
- Easy degree. At the initial stage of the disease, the patient may not attach importance to slight reddening of the gums or uncomfortable sensations in the oral cavity. Thorough brushing or other preventive measures prevent the spread of inflammation to other parts of the gums.
- Medium degree. If you ignore the first symptoms, bleeding, swelling of the tissues appears, inflammation spreads over large areas.
- Severe degree. Acute gingivitis occurs due to prolonged exposure to adverse factors. The result can be hyperplasia, necrotic changes in the gum tissue.
By the nature of the inflammatory process, there are:
- Catarrhal gingivitis. The easiest and most common form of gingivitis of the oral cavity. It is characterized by swelling of the tissues, bleeding, redness or cyanosis of the gums. With a sharp exacerbation and refusal of treatment, extremely severe symptoms develop, hyperthermia and a transition to the chronic form of catarrhal gingivitis are observed.
- Hypertrophic gingivitis. The initial stage of development of hypertrophic gingivitis can manifest itself only as a slight swelling without noticeable redness or other symptoms. Only a dentist can establish the appearance of the disease at this stage. As the inflammation progresses, thickening, keratinization of the epithelium, significant hyperplasia of the mucous membrane of the gum, growing tissue protrudes from the top of the tooth, making it difficult to chew, performing hygienic procedures, and tartar grows under the gum. There is bleeding, pain when brushing your teeth or eating food.
- Ulcerative necrotic gingivitis. Also known in dentistry under the name "Plauta-Vincent's gingivitis." This type is characterized by the appearance of erosion, ulceration and necrotic areas on the mucous membrane of the gums. The clinical picture is complemented by soreness, purulent discharge, bleeding, bad breath. The general condition worsens: weakness appears, body temperature rises, a noticeable increase and compaction of regional lymph nodes occurs.
If ulcerative gingivitis is not treated promptly, irreversible tissue destruction, development of abscesses, blood poisoning, and even death are possible.
- Atrophic gingivitis. It is characterized by a dystrophic change in epithelial tissue, a decrease in the volume of the gums, and a gradual opening of the neck of the tooth. The patient experiences pain when eating, drinking cold or hot drinks. This type of gingivitis most quickly turns into periodontitis.
Diagnosis and treatment of gingivitis
The appointment of a treatment course is preceded by a diagnosis by a dentist or periodontist. Symptoms of gingivitis, the presence of plaque or stone, as sources of bacterial infection, can be detected at a routine examination of the oral cavity.
Therapeutic measures when establishing a diagnosis of gingivitis are prescribed by the dentist and begin by finding out the cause of the appearance and determine the severity of the inflammatory process. How to treat gingivitis can be prescribed by a dentist or periodontist.
Depending on the type, stage and causes of the disease, different principles of anti-inflammatory therapy at home or in the dental office are possible. Gingivitis in the mild form or at the initial stage is treated quite successfully.
Drug therapy
First of all, you need to replace the toothbrush with a new one, and the toothpaste with an antibacterial one. To the hygienic procedures add rinsing of the oral cavity using solutions containing chlorhexidine, furatsilin, methyl salicylate.
The use of special complex ointments and creams containing antibacterial, anti-inflammatory and analgesic components gives good results. These include medicines:
- Metrogil Dent.
- Kamistad.
- Holisal.
Acute gingivitis, the treatment of which should begin immediately after diagnosis, can lead to relapse with poor-quality therapeutic measures. Nonsteroidal anti-inflammatory drugs: Ibuprofen, Nimesulide help to treat toothache with gingivitis.
Some forms of gingivitis require mandatory medical supervision of treatment or the help of a dentist. If tartar is found, which is a favorite place for the development of pathogenic microorganisms, it is necessary to remove it in a dental clinic.
Treatment of ulcerative necrotic gingivitis must be carried out under the supervision of a doctor who will select the appropriate antibiotic therapy. Hypertrophic and atrophic gingivitis require surgical intervention to correct the shape of the gingival margin. Gingivoplasty or gingivectomy is performed as indicated by a periodontic surgeon.
Folk remedies for gingivitis
Folk remedies in the treatment of gingivitis show good results and can alleviate the condition even with severe forms or types of gingival inflammation. A decoction of chamomile, calendula flowers, sage is prepared at the rate of 1 tbsp. l 200 ml of boiling water. Such infusions have anti-inflammatory and valuable regenerative effects. It is necessary to apply them in the form of rinses of the oral cavity several times a day, especially after eating, before going to bed.
Beekeeping products are widely used in the treatment of gingivitis: natural honey (applied to the gums), propolis (used for rinsing).
Vitamin therapy in the treatment of gingivitis is aimed at strengthening the body's immune defenses, replenishing the reserves of vitamins involved in tissue regeneration. Calcium preparations, vitamin, mineral complexes, vitamins C, A, E with gingivitis will help relieve gum inflammation and accelerate the healing process.
Important! Without visiting a specialist, you can independently eliminate the symptoms, but not the cause of gingivitis. Therefore, if a disease is detected, it is recommended to contact a medical institution.
Gingivitis Prevention
Gingivitis refers to those diseases of the oral cavity that are easier to prevent than to cure. Preventive measures aimed at preventing the development of inflammation include:
- Quality care for the company cavity. The key to success is the use of an individual toothbrush, the regularity and thoroughness of hygiene procedures, and brushing before bedtime.
- The use of mouthwash, the antiseptic properties of which will help maintain the balance of microflora. It is advisable to use it after each meal.
- Application for cleaning interdental space of special dental floss. They help to remove all food particles that are not touched by the toothbrush, thereby preventing the development of microorganisms in the interdental space.
- A regular visit to the dentist at least once every six months.
- Treatment of carious teeth and other sources of infection in the body.
- Quitting smoking, drinking alcoholic beverages.
- A complete balanced diet with enough foods containing vitamins and minerals.
The main prevention of gingivitis instills in children a responsible attitude to oral care, and forms an understanding of the importance of regular visits to the dentist.
Good oral hygiene is the principle of preventing the development of gingivitis and other gum inflammations.
The effects of gingivitis
Gingivitis is an extremely unpleasant disease, which, with its manifestations, worsens the patient's quality of life. Painful sensations in the oral cavity, bleeding gums, bad putrid breath negatively affect the appetite, cause an aversion to food and drinks, affect communication with people.
One of the dangers of the disease is that causes of gingivitis with untimely elimination can give impetus to the development of a more severe form of gum disease - periodontitisin which there is a destruction of the tooth-gingival attachments, loosening and tooth loss is possible.
Acute and chronic gingivitis require a timely and high-quality treatment course under the supervision of a specialist dentist or periodontist.